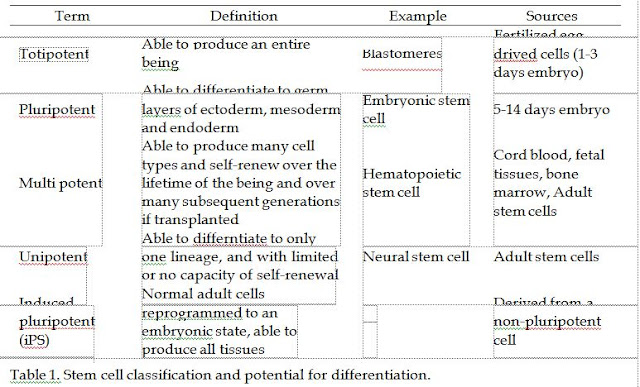
Embryonic stem cells (ESCs) are able to produce all tissues and germ lines (sperm and eggs) and to self-renew indefinitely. These pluripotent stem cells were first isolated in 1998. However, the resources of ESCs are limited, and since human embryos have to be destroyed for ESC production, many people oppose the use of this kind of stem cell for scientific research or therapeutic approaches.
ESCs can be produced in the laboratory in two ways: by derivation from the inner cell mass (ICM) of a blastocyst in a 5-14 days embryo, or by somatic cell nuclear transfer (SCNT). SCNT or cloning, which was brought into public attention after cloning of the sheep "Dolly" in 1997 (Wilmut et al., 1997), is also used as a technique to produce stem cells for basic developmental biology research and cell-based therapies. Through cloning, the DNA of an unfertilized egg is replaced with the DNA of the patient's cell. Although a Korean scientist claimed to extract stem cells from human cloning in 2004 (Hwang, 2004, 2005), his work was recognized as a scientific fraud later on (Kennedy, 2006). Although there are important concerns about the safety of cloning, as Fischbach and Fischbach state, stem cells produced by therapeutic cloning have the advantage over those harvested from embryos resulting from IVF or aborted foetuses in that the cells generated through therapeutic cloning are genetically similar to the cells of the individual who donated the nucleus (Fischbach & Fischbach, 2004), therefore they are immunologically matched to the patient, which avoids problems of rejection (Coors, 2002; Weissman, 2002). Another source of pluripotent cells are human embryonic germ (hEG) cells which are derived from the gonadal ridges of aborted fetuses (Gogle et al., 2003; Balint, 2001).
Multipotent stem cells have a research history of more than 40 years and have been successfully used for treatment of some disorders such as leukaemia for decades (Hyne,
2008). The use of these stem cells is surrounded with less ethical and religious debate since they can be naturally found as adult stem cells throughout the body; however, their limited potential of differentiation has restricted their practical uses. Also, mass production of multipotent (and unipotent) stem cells is time consuming.
Inactive adult stem cells (SCs) exist in many tissues and need to be signalled.
Haematopoietic SCs, which are used for bone marrow transplantation in oncology, are a good example of the use of this kind of SCs in cell and tissue transplantation. Medical waste, such as amniotic fluid, placenta, menstrual blood, synovial fluid from knee, teeth, liposuction aspirate, umbilical cords, is a source of adult stem cells (Lewis, 2009).
Induced pluripotent stem (iPS) cells have been reprogrammed with retroviruses to behave
like embryonic stem cells (Hyne, 2008). The methods that reprogram adult human cells to a pluripotent state were described firstly by two groups of researchers from Japan and the United States (Takahashi et al., 2007; Blow, 2008). Considering the mutagenicity of the viruses and the potential to activate oncogenes, and the debate on their properties and potential as embryonic stem cells, iPS cells are not used as a practical therapeutic agent yet (Blow, 2008). Further experiments showed that reprogramming genes can be done in safer ways without the use of viruses (Lewis, 2009).
The main potential use of stem cells in medicine is for cell and tissue replacement therapies. There are hopes for lifelong treatment of disorders such as Huntington’s disease, Parkinson’s disease, type 1 diabetes mellitus, myocardial infarction, spinal cord injuries, stroke, chronic skin ulcers and burns by transplantation of stem cells. The utilization of stem cells in the treatment of Alzheimer’s disease, avascular necrosis, neural deafness,
osteoarthritis, liver failure, and some autoimmune disorders including multiple sclerosis (MS), rheumatoid arthritis, and systemic lupus erythematosus (SLE) is also under research. Stem cell research may pave the way for designing novel approaches in regenerative medicine. Since ESCs can proliferate without limit and can differentiate to any cell type, they offer unprecedented access to tissues from the human body, and they have the potential to provide an unlimited amount of tissue for transplantation therapies to treat a wide range of degenerative diseases (National Institute of Health [NIH], 2006). Genetic research, understanding of normal development, research on the differentiation of human tissues, and birth defects investigations are other potential uses of stem cells. Stem cells can be used for drug development and toxicity tests too. They can support research on safety and efficacy of new drugs.
The therapeutic potential of stem cells has been publicized, and much related public enthusiasm has been reflected in some stories and movies. There are scientific, ethical, legal, religious, and social challenges for the use of stem cells for cell and tissue transplantation. The concerns should be addressed before the widespread use of this science and technology. We intend to review main ethical issues and religious perspectives in the following sections.
0 comments:
Post a Comment